Researchers use 3D printing to aid human face transplants

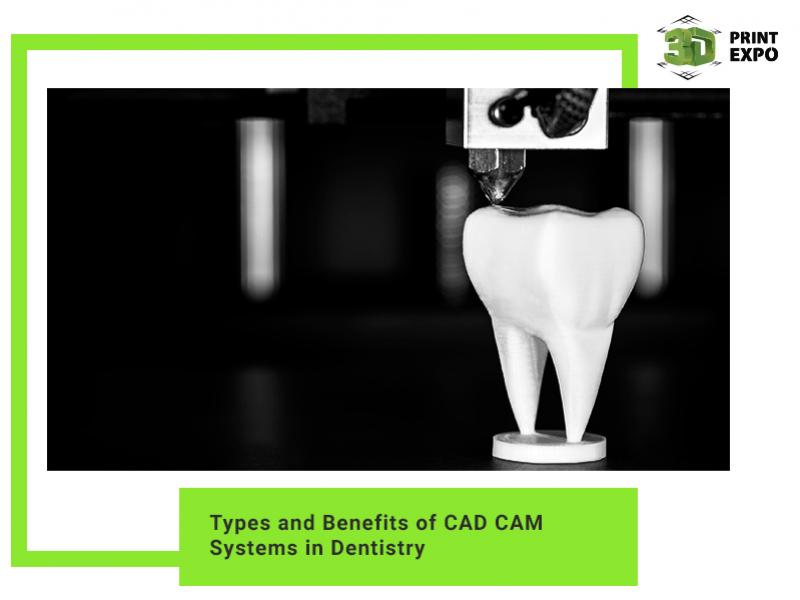
Surgeons are using computed tomography (CT) and highly accurate 3D printers to recreate life-size models of patients' heads to guide face transplantation surgery, according to a study presented today at the annual meeting of the Radiological Society of North America (RSNA).
"This is a complex surgery and its success is dependent on surgical planning," said Frank Rybicki from Brigham and Women's Hospital in the US. "Our study demonstrated that if you use this model and hold the skull in your hand, there is no better way to plan the procedure."
"In some patients, we need to modify the recipient's facial bones prior to transplantation," said Amir Imanzadeh, research fellow from the Brigham and Women's Hospital. "The 3D printed model helps us to prepare the facial structures so when the actual transplantation occurs, the surgery goes more smoothly."
Physicians at Brigham and Women's Hospital in Boston performed the country's first full-face transplantation in 2011 and have subsequently completed four additional face transplants. The procedure is performed on patients who have lost some or all of their face as a result of injury or disease.
In the study, the researchers assessed the clinical impact of using 3D printed models of the recipient's head in the planning of face transplantation surgery.
Each of the transplant recipients underwent preoperative CT with 3D visualization. To build each life-size skull model, the CT images of the transplant recipient's head were segmented and processed using customized software, creating specialized data files that were input into a 3D printer.
Although the entire transplant procedure lasts as long as 25 hours, the actual vascular connections from the donor face to the recipient typically takes approximately one hour, during which time the patient's blood flow must be stopped.
"If there are absent or missing bony structures needed for reconstruction, we can make modifications based on the 3D printed model prior to the actual transplantation, instead of taking the time to do alterations during ischemia time," Dr. Rybicki said. "The 3D model is important for making the transplant cosmetically appealing."
The researchers said they also used the models in the operating room to increase the surgeons' understanding of the anatomy of the recipient's face during the procedure.

"You can spin, rotate and scroll through as many CT images as you want but there's no substitute for having the real thing in your hand," Dr. Rybicki said. "The ability to work with the model gives you an unprecedented level of reassurance and confidence in the procedure."
Senior surgeons and radiologists involved in the five face transplantations agreed that the 3-D printed models provided superior pre-operative data and allowed complex anatomy and bony defects to be better appreciated, reducing total procedure time.
"Less time spent in the operating room is better for overall patient outcomes," Dr. Pomahac added.
Based on the results of this study, 3D printing is now routinely used for surgical planning for face transplantation procedures at Brigham and Women's Hospital, and 3D printed models may be implemented in other complex surgeries.